Category: Filler injection
-

Volumetric Effect and Patient Satisfaction after Facial Fat Grafting
Background: Facial fat graft decreases in volume after transplantation. This observation is based on overall facial three-dimensional analyses, because there is sparse information on volume changes in well-defined aesthetic areas. The authors aimed to assess the overall and, more specifically, the local volumetric effects of facial fat grafting and relate these effects to patient satisfaction…
-

Under Eye Filler Before And After Photos❤
What is under eye filler? A tear trough is a deep crease between the lower eyelid and upper cheek, and as we age we can experience volume loss in this area which can leave dark circles, shadows and hollows around the delicate under-eye area. This can often make us look tired, older, haggard and run…
-
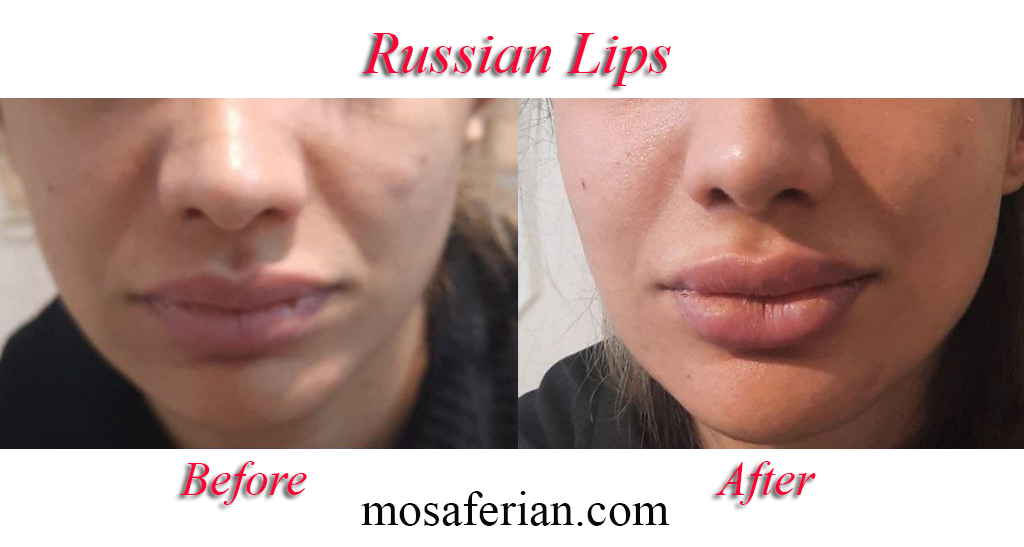
Russian Lip Filler Before And After💋
What is russian lip filler? This new trend has introduced a brand new shape to the lips, providing a flatter, wider look to match the one supported naturally by Russian women. The trend began due to the desire for lips that are larger in volume and plumpness, without the worry of filler migration or the…
-

Arnica Cream For Bruises In 2024🌻
Arnica cream seems to have a mitigating effect on ecchymosis, most notably following rhinoplasty and facelifts/facial procedures. Bromelain is well supported across numerous studies in reducing trismus, pain, and swelling following molar extractions. However, there was no effect demonstrated when evaluating topical arnica following blepharoplasty procedures. Arnica cream known to have anti-inflammatory, antimicrobial, and analgesic…
-
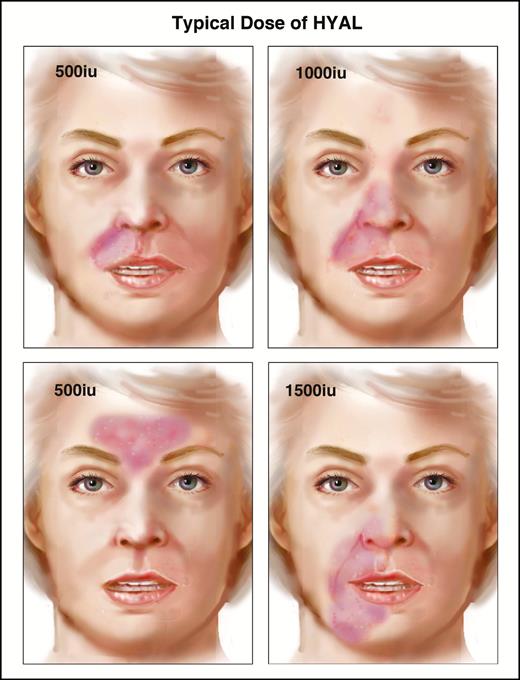
Hyaluronidase protocol for dermal fillers
New High Dose Pulsed Hyaluronidase Protocol for Hyaluronic Acid Filler Vascular Adverse Events Claudio DeLorenzi, MD, FRCS The purpose of this article is to update the changes to the author’s protocols used to manage acute filler related vascular events from those previously published in this journal. For lack of a better term, this new protocol…
-

Non surgical nose job before and after
What is a non surgical nose job and how does it differ from a traditional nose job? Traditionally, a rhinoplasty is a surgery that changes the shape of the nose. It requires anesthesia and considerable healing time because of bruising and swelling, but the results are permanent. On the other hand, a liquid nose job…
-

❤THE MAGIC OF TEAR TROUGH CORRECTION BEFORE AND AFTER PHOTOS IN 2024
What is tear trough correction? The tear trough ligament, as well as other retaining ligaments, like orbicularis retaining ligament, and zygomatic cutaneous ligament, plays an important role on the facial contour during aging process. They can be released partially through non-surgical approach as a first step to eliminate the tear trough. Tear trough ligament…
-

Hyaluronidase injection to remove filler❤
What is hyaluronidase? Hyaluronidase is a natural substance found in the body, which is collected from either cows or pigs. It is cleaned up to remove animal substances. It may also be produced in a laboratory that recreates it from human albumin sources. This product is routinely used for reversing hyluronic acid fillers such as…
-

Chin augmentation before and after
Chin implant or augmentation Chin implant needs surgery that always carries inherent risks including scarring, infection, and anesthesia complications. Surgical chin enhancement involves inserting a chin implant. This implant can, rarely, move after surgery, having to be re-positioned. If there is a significant infection after surgery, the implant must be removed. In both of these…
-

Lip Augmentation Before And After Photos👄
What is lip augmentation? Lip augmentation is a procedure to provide more fullness to the lips and improved shape. It can be performed in patients who have innately thin lips or in patients who have lost lip volume from the aging process. Four techniques are more commonly utilized: Alloderm Fat grafts or injection Dermal/fat injection…
